
The ongoing series on by ProPublica has shined light on the serious problem of US maternal mortality. Interestingly the series evolved over time, initially framing the problem with a story of a privileged white woman who was a victim of malpractice and ultimately recognizing that it is a problem of race and healthcare disparities.
Perhaps the most shocking fact about US maternal mortality is this:
…[A]lthough Washington, DC, has the highest maternal mortality ratio in the nation, non-Hispanic white patients in this district have the lowest mortality ratio in the United States. Excellent care is apparently available but is not reaching all the people.
New data presented in the forthcoming issue of Obstetrics and Gynecology confirms this assessment. The paper is Health Care Disparity and Pregnancy-Related Mortality in the United States, 2005–2014.
[pullquote align=”right” cite=”” link=”” color=”” class=”” size=””]Excellent obstetric care is available but it is not reaching the women who need it most.[/pullquote]
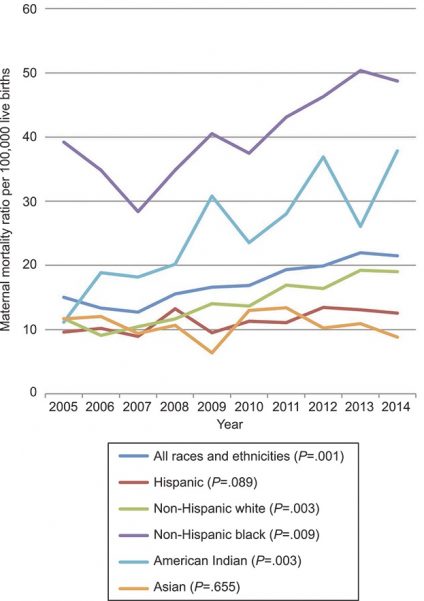
The trend is displayed in the following graph: Trends in maternal mortality ratio (maternal deaths/100,000 live births) by ethnic group and race: United States, 2005–2014. Numbers in parentheses represent P values for the Jonckheere-Terpstra test.Moaddab.
The authors note:
The U.S. maternal mortality ratio continues to climb and reached a rate of 21–22 per 100,000 in 2013 and 2014. Many explanations for this trend have been offered. Although the United States has a higher rural population than many European nations … our data failed to identify a statistical correlation between state-specific maternal mortality and either rural status or poverty. Immigration has also been cited as a factor in this mortality trend. However, we found lower mortality for Hispanic women who make up the majority of recent immigrants.
So the cause is NOT rural status, immigration or poverty.
What about the C-section rate, the all purpose bogeyman constantly used by natural childbirth advocates to scare women about obstetric care?
The high U.S. cesarean rate has also been invoked as an explanation for increased mortality, yet our data demonstrate only a weak correlation of mortality with cesarean delivery. Furthermore, previous work has demonstrated that this correlation does not reflect causation; the overwhelming majority of maternal deaths associated with cesarean delivery is a consequence of the indication for the cesarean delivery, not the operation itself.
What accounts for the difference in statewide maternal mortality rates?
Our data suggest that much of the variation in statewide maternal mortality ratios in the United States is accounted for by social rather than medical or geographic factors: unintended pregnancy, unmarried mother, and non-Hispanic black race. These data provide evidence for a strong contribution of racial disparity to maternal mortality ratio in the United States. Particularly striking is the close correlation between ethnic background and maternal mortality. A factor derived from factor analysis, which primarily represented ethnic background, accounted for 26% of the differences in statewide mortality. Excellent care is apparently available, but is not reaching all the people.
How should we compare maternal mortality across states (or countries, though the authors do not address international differences)?
…[C]omparative health care statistics that do not adjust for these important demographic factors are of little significance in judging the intrinsic quality of available health care in an individual state or region. The potential relative contributions of factors such as racial disparities in health care availability and access or utilization by underserved populations are not addressed by our data, but are important issues faced by states seeking to decrease maternal mortality. Ethnic genetic differences may also be involved. In addition, the potential role of unconscious (implicit) bias in this significant racial disparity must be considered.
Indeed, the US, which has the highest maternal mortality of any industrialized nation has by far the highest proportion of women of African descent.
The British press has been bemoaning the high US maternal mortality rate. For example, a recent BBC interview with Serena Williams was described thus:
Serena Williams says it is “heartbreaking” black women in the United States are more likely than white women to die from complications in pregnancy or childbirth.
It IS heart breaking that black women in the US are 3X more likely to die from complications in pregnancy or childbirth. What the BBC and Serena Williams don’t seem to realize is that the disparity is even greater in the UK; black women in the UK are 4X more likely to die from complications in pregnancy or childbirth.
According to the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2013–15:
The rates of maternal mortality varied by age, socioeconomic status and ethnic background of the women, which are known to be independently associated with an increased risk of maternal death in the UK. The rate of maternal mortality was higher amongst older women, those living in the most deprived areas and amongst women from particular ethnic minority groups… Comparable to the previous reports, the risk of maternal death in 2013–15 was signi cantly higher among women from Black ethnic minority backgrounds compared with White women (RR 4.28; 95% CI 2.65 to 6.69).
The overall UK statistics look better than the US because women of African descent represent a far smaller proportion of the population in the UK (3%) than in the US (12.85%). The sad truth is that lower rates of maternal mortality in other industrialized countries reflect the fact that those countries are whiter. The countries with the lowest maternal mortality rates in the world (including Iceland, Sweden, Finland and Japan) are the whitest countries in the world.
The authors conclude:
…The increased mortality ratios seen in the United States in recent years reflect significant social as well as medical challenges and are closely related to lack of access to health care in the non-Hispanic black population. Our results provide evidence for the strong contribution of racial disparity to the maternal mortality ratio in the United States and suggest that addressing issues related to health care disparity and access for this population will play an important role in national attempts to reverse this mortality trend.
The only question that remains is whether we have the will to tackle the problem.

