Ever notice how midwives can’t seem to write a paper that does not involve shilling for midwifery jobs?
The latest series on midwifery in The Lancet is no exception. The entire focus of the series is on midwives and their employment opportunities, not on women and babies and their needs.
It’s all the more remarkable when you consider the series of stunning midwifery failures in industrialized countries.
Multiple studies in The Netherlands, the country with the highest proportion of homebirths, have shown that Dutch perinatal mortality is among the highest in Europe. Moreover, Dutch midwives caring for low risk patients have a HIGHER perinatal mortality rate than Dutch obstetricians caring for HIGH risk patients. That is an incredible indictment of midwifery.
Over in the UK, the situation is so dire that the government has released a scathing report:
The Health Service Ombudsman examined the supervision of midwives after a series of reports into a scandal at University Hospitals of Morecambe Bay Foundation trust involving the deaths of 14 babies and two mothers…
The damning report is fiercely critical of subsequent investigations into the deaths by the trust and the local health authority – which it found guilty of “maladministration” for failing to properly probe the deaths.
Under the current NHS system of regulation, local midwives in were asked to investigate their peers following a series of deaths at Furness General Hospital.
Despite clear evidence of serious mistakes made, they found their colleagues did nothing wrong.
There were long delays investigating the deaths, and failures to highlight obvious lapses in care – such as babies not having their heart rates monitored and not being given antibiotics despite being very poorly, the report found.
Not surprisingly, the amount of money paid for bad outcomes and the cost of insurance coverage have skyrocketed in the wake of midwifery incompetence. Indeed, a fifth of maternity funding is spent on insurance.
Australia has had its own problems with midwives, and the US has an entire second class of midwives (CPMs) who are grossly undereducated and undertrained and leave a trail of tiny dead bodies in their wake.
Yet as far as I can tell, there has not been a single paper in any midwifery journal investigating the deadly lapses or suggesting stricter standards and greater midwifery accountability.
In contrasts, midwives in general, and midwifery papers in particular, are constantly shilling for midwife employment opportunities.
The new papers in The Lancet appear to be no exception. The focus of the series is squarely on midwives and their employment opportunities, NOT on women and their babies.
The first sentence sets the tone:
Midwifery matters more than ever
That is complete and utter bullshit.
Women and babies have been dying in droves since the beginning of recorded history. Traditional midwives tried, but were not able to do much to stem the tide. ONLY modern obstetrics has been successful in saving lives. Indeed it has been spectacularly successful, saving literally millions of lives each and every year around the world.
Too many women and babies continue to die for lack of obstetric care. The solution is more hospitals, more obstetricians, more medications, more interventions in general, and more C-sections in particular. Well trained midwives, as avatars of modern obstetrics, have an important role to play in providing obstetrical services. They are not the solution to the problem, nor should their employment goals be a focus of a series.
Look at the following list of key findings from the series:
• These findings support a system-level shift, from maternal and newborn care focused on identification and treatment of pathology, to a system of skilled care for all, with multidisciplinary teamwork and integration across hospital and community settings.Midwifery is pivotal to this approach.
• Future planning for maternal and newborn care systems in low-income and middle income settings can benefit from using the evidence-based framework for qualitymaternal and newborn care (QMNC) for workforce development and resource allocation.
• The views and experiences of women themselves, and of their families and communities, are fundamental to the planning of health services in all countries.
• Midwifery is associated with more efficient use of resources and improved outcomes when provided by midwives who are educated, trained, licensed, and regulated, and midwives are only effective when integrated into the health system in the context of effective teamwork and referral mechanisms and sufficient resources.
• Promoting the health of babies through midwifery means supporting, respecting, and protecting the mother during the childbearing years through highest quality care; strengthening the mother’s capabilities is essential to longer term survival and wellbeing for the infant.
• Strengthening health systems, including building their workforce, makes the difference between success or reversal in maternal and newborn health. Since 1990, the 21 countries most successful in reducing maternal mortality rates—by at least 2·5% a year—have had substantial increases in facility-birthing, and many have done this by deploying midwives.
• Effective coverage of reproductive, maternal, and newborn health (RMNH) care requires three actions. These are: facilitating women’s use of midwifery services, doing more to meet their needs and expectations, and improving the quality of care they and their newborn infants receive.
• Although evidence from more settings is needed, evidence so far shows that midwifery care provided by midwives is cost-effective, affordable, and sustainable. The return on investment from the education and deployment of community-based midwives is similar to the cost per death averted for vaccination.
• Quality improvements in RMNH care and increases in coverage are equally important for achieving better health outcomes for women and newborn infants. Investment in midwives, their work environment, education, regulation, and management can improve the quality of care in all countries.
• Efforts to scale up QMNC should address systemic barriers to high-quality midwifery— eg, lack of understanding of midwifery is and what it can do, the low status of women, interprofessional rivalries, and unregulated commercialisation of childbirth.
More bullshit!
A system-level shift, from maternal and newborn care focused on identification and treatment of pathology to a system of skilled care for all? Why on earth would be turn our focus from the mothers and babies dying of pathological conditions to a system that gives greater emphasis to women who don’t need life saving care?
To increase employment opportunities for midwives, mothers and babies be damned.
The typical woo-mongering of midwives is given pride of place. Women and babies are dying hideous deaths, but midwives want to talk about “strengthening the mother’s capabilities.” (For what? They don’t say.) There’s a lot of talk about “respecting” mothers, investing in midwifery, integrating midwifery more fully into healthcare, reducing interprofessional rivalries and stopping the “commercialisation” of childbirth, EXCEPT when it is midwives who are doing the commercializing.
They seem to be entirely ignoring the actual causes of maternal and perinatal mortality.
According to the World Health Organization, the leading causes of maternal death are:
- severe bleeding (mostly bleeding after childbirth)
- infections (usually after childbirth)
- high blood pressure during pregnancy (pre-eclampsia and eclampsia)
complications from delivery- unsafe abortion
What can midwives do about these problems? Not much.
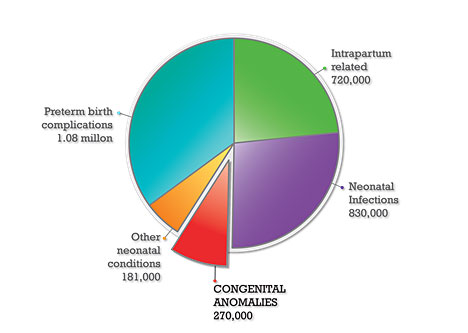
According to the WHO, the leading causes of neonatal death are:
- prematurity
- infection
- intrapartum events (asphyxia, shoulder dystocia, etc.)
- congenital anomalies
What can midwives do about these problems? Not much.
Indeed the report itself provides only paltry evidence that increasing midwifery services will have an impact on these problems.
What do women and babies really need?
They need access to forceps, vacuums, C-sections, D&Cs for miscarriages, surgical services for ruptured ectopics, and skilled surgeons capable of repairing obstetric fistulas.
They need access for medications like anti-seizure meds for eclampsia, Cytotec for obstetric hemorrhage, antibiotics for infections, Rhogam to prevent erythroblastosis fetalis, Vitamin K to prevent hemorrhagic disease of the newborn.
They need access to contraception and pregnancy termination so women can control their own fertility.
They need more obstetricians to supervise midwives, care for patients, and provide care that midwives are incapable of providing. They need more MEDICAL facilities to care for every aspect of women’s and children’s health, NOT birth centers which care only for childbirth related issues.
They need more neonatologists to save premature babies, more neonatal intensive care units, and more supplies with which to run them.
But midwives cannot provide these services, so who cares?
The Lancet series on midwifery is an extended advertisement for midwifery services, despite the fact that those are not the primary services needed.
I have a question for the folks at The Lancet:
Now that midwives have been allowed to run their giant ad, when can we expect to see a series on what women and babies need, as opposed to merely what midwives can provide?