If you want to understand the gulf that separates natural childbirth advocates from obstetricians, check out the latest midwifery and obstetric journals. No, none of this month’s issues have a paper about the difference. Rather, it is the type of papers in each that illustrate the difference.
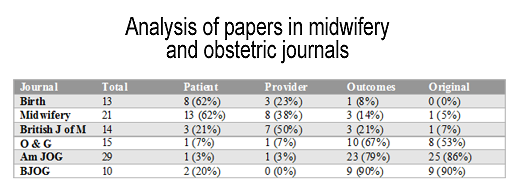
Let’s start with the natural childbirth journal Birth, published by Lamaze International. There are 13 articles and reviews in the September issue: 8 are about the patient experience of childbirth, 3 are concerned with the provider experience and beliefs, only 1 is focused on safety outcomes for babies or mothers, and none contribute original knowledge.
Contrast that with the September issue of Obstetrics and Gynecology. There are 15 obstetrics articles: of these, 1 is about the patient experience, 1 is potentially concerned with provider experience and beliefs, 10 are focused on safety outcomes for babies and mothers, and 8 contribute original knowledge (each article can be counted in more than one category).
In other words, the vast majority of articles in Birth focuses on patient or provider experience, only 1 paper focused on actual outcomes for mother and or baby and there was no research that contributed to the body of scientific evidence about obstetric practice. In Obstetrics and Gynecology, the proportions were reversed. The majority of articles focused on safety outcomes for mothers and or babies and more than half contribute original knowledge to the body of scientific evidence about obstetric practice. Only 1 article focuses on patient experience, and one potentially focuses on provider experience.
These findings extend to other midwifery and obstetric journals. Below is a table with the results of an informal analysis of the latest issues of the 3 most prominent midwifery journals and the 3 most prominent obstetric journals. (In addition to Birth and Obstetrics & Gynecology, they include Midwifery, the British Journal of Midwifery, the American Journal of Obstetrics and Gynecology, and the British Journal of Obstetrics and Gynecology.
Of note, the proportions do not add up to 100% because an article can be counted in more than one category (eg. safety outcomes and original knowledge).
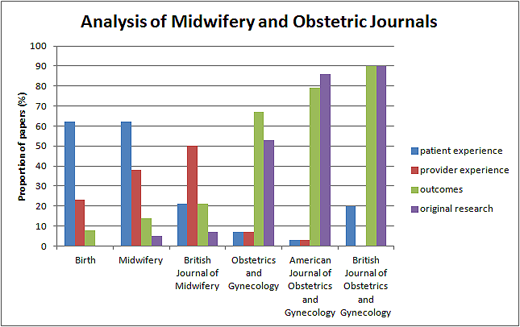
A bar graph of the same data expresses the difference even more dramatically.
What is striking to me is how little midwifery research is concerned with safe outcomes. All of the midwifery journals devote a proportion of 20% or smaller to safe outcomes. Presumably that is not because midwives and natural childbirth advocates don’t care about childbirth culminating in a healthy mother and healthy baby. I suspect that the reason for the bizarre lack of interest in safe outcomes is two fold. First, midwives and natural childbirth advocates see no reason to even think about women who are high risk. If they are outside the scope of practice, these women are simply ignored. Second, midwives and natural childbirth advocates appear to assume that low risk women will nearly always have safe outcomes. That, of course, is a serious problem, since childbirth is inherently dangerous, even for women who are low risk. Midwives and natural childbirth advocates can pretend that the dangers don’t exist because they have been virtually eliminated by the interventions of modern obstetrics, the very interventions that they deplore.
Simply put, the real difference between natural childbirth advocates and obstetricians is that natural childbirth advocates live in a fantasy world of their own construction. In that fantasy world, childbirth is always safe, so there is no reason to ever worry about safety. Hence midwifery journals are filled with articles obsessing about whether women had IVs or midwives enjoyed themselves at their patients’ births. Obstetricians, in contrast, live in the real world, where low risk women can and do routinely have life threatening complications. Their priority is safe childbirth: healthy babies and healthy mothers.