Benjamin Disraeli famously said, “There are three kinds of lies: lies, damned lies and statistics.”
Midwife Hannah Dahlen, in her ongoing efforts to blacken the reputation of obstetricians, corroborates Disraeli’s claim. Her latest paper, Rates of obstetric intervention among low-risk women giving birth in private and public hospitals in NSW: a population-based descriptive study, published in the current issue of the British Medical Journal Open edition has, is a master class in lying with statistics.
The primary conclusion of the paper is:
Over the past decade these interventions have increased by 5% for women in public hospitals and by over 10% for women in private hospitals. Among low-risk primiparous women giving
birth in private hospitals 15 per 100 women had a vaginal birth with no obstetric intervention compared to 35 per 100 women giving birth in a public hospital.
The part of the study that is generating media attention is:
TENS of thousands of Australian women with low risk of birth complications are undergoing unnecessary medical interventions in private hospitals in a trend that a leading midwifery expert has described as ”horrifying”.
Indeed, the authors of the paper state:
The continual rise in obstetric intervention for low-risk women in Australia is concerning in terms of morbidity for women and cost to the public purse. The fact that these procedures which were initially life-saving are now so commonplace and do not appear to be associated with improved perinatal death rates demands close review.
There is just one teensy, weensy problem with the paper:
The authors never looked at the perinatal death rate in the population that they studied so they literally have no idea of the impact of the interventions they decry. They performed a bait and switch; they looked at intervention rates in a low risk population and compared them to mortality rates in the overall population including high risk women, prematurity and all complications of pregnancy.
Let’s look at the population they studied, women from the Australian state of New South Wales:
The ‘standard primipara’ is defined as a primiparous woman aged 20–34 years, who had no pre-existing or pregnancy-related medical conditions, gave birth at 37–41 weeks gestation to a fetus in a cephalic presentation within the 10th and 90th centiles for birth weight. The ‘standard multipara’ was a multiparous woman aged 20–34 years, who had no pre-existing or pregnancy related medical conditions, gave birth at 37–41 weeks gestation of a fetus in a cephalic presentation within the 10th and 90th centiles for birth weight. In both definitions we included ‘non smoking’.
That yielded a study population of 124,431 women:
… 30 152 low-risk primiparous women who gave birth in a private hospital and the 94 279 low-risk primiparous women who gave birth in a public hospital.
But when it came time to compare the intervention rates to the mortality rate, the authors used the perinatal mortality rate from 691,738 births during the period 2000–2008. In other words, the perinatal death rate includes 567,307 women that aren’t in the study. In other words 82% of the mothers from whom the mortality rates are derived AREN’T in the study. Those are the women with high risk conditions, prematurity and pregnancy complications, and, of course, most of the perinatal deaths occur in that group.
Even then, the authors play fast and loose with the truth:
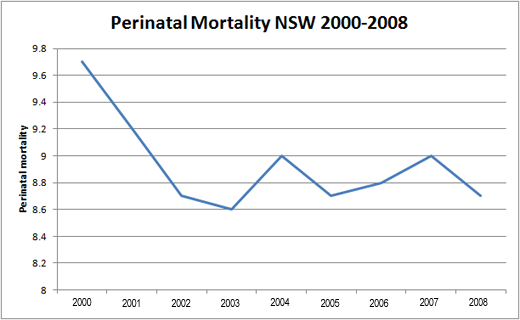
The NSW rate of perinatal mortality was between 8.6 and 9.6 per 1000 births between 2000 and 2005 and between 8.7 and 9 per 1000 births between 2005 and 2009.
That’s a rather curious way to describe a trend over time, but it sounds a lot better for Dahlen’s purposes than an accurate report of the information: from 2000-2008, overall perinatal mortality in New South Wales dropped from 9.7/1000 to 8.7/1000, a drop of 10%.
How did the reviewers let this bait and switch go by. BMJ Open provides the names and comments of the reviewers. The reviewers for this paper are two midwifery professors Meredith McIntyre, who researches “midwifery care reform” and Maralyn Foureur, a colleague of one of the authors on another publication, who researches “ways to keep birth normal.” In other words, to professional colleagues of the authors known to be in agreement with their views about interventions. There was no review by an obstetrician or a statistician.
One of the reviewers does note that in the original manuscript, the authors attempted to use perinatal mortality rates from Australia as a whole:
The national rate of perinatal mortality rather than the NSW state rate is used in the Discussion. It is more appropriate to use the NSW rate in order to better support your argument that the increase in interventions for private women does not result in improved benefits for babies…
She’s only half right. It is indeed inappropriate to use the national perinatal mortality rate, but it is also inappropriate to use the NSW rate of perinatal mortality. The correct comparison would require the use of the perinatal mortality rates in the group of low risk women under study.
The BMJ ought to re-evaluate the way that it reviews papers. Professional colleagues allies of the authors should not be used as reviewers, claims about obstetric interventions should be reviewed by obstetricians, and statistics claims should be reviewed by statisticians.
The bottom line is that this study tells us only the trend of intervention use among low risk women in NSW from 2000-2008 and the difference in intervention rates between low risk women in private and public hospitals. That’s all it can tell us. There is no information presented that would allow us to draw conclusions about whether the interventions were used appropriately or whether they led to a decrease in perinatal mortality.
In contrast to Ms. Dahlen’s claims, what is “horrifying” here is not the increase in interventions, but the bait and switch used in the attempt to advance the midwifery objective of blackening the reputation of modern obstetrics.