Imagine if someone wrote an article entitled, What is the Evidence for Treating Chest Pain in Healthy Men? and claimed:
There is no evidence that hospitalization for chest pain in men improves outcome.
Makes it sound like there is no reason for a man to worry if he has chest pain, no reason to call 911, no reason to take an aspirin, no reason to do anything, doesn’t it?
That’s what most people would take away from the article, even if they read the caveat.
There is no evidence that hospitalization for isolated chest pain in otherwise healthy men has any beneficial impact. Based on the lack of evidence, any recommendation for hospitalization for chest pain with no other symptoms, no underlying risk factors, no complicating conditions, and normal test results is a weak recommendation based on clinical opinion alone.
Okay, now it’s clear. The article is actually talking specifically about chest pain that has already been determined to be unrelated to any cardiac issues. Well, duh! No one ever claimed that every episode of chest pain was a heart attack, but that doesn’t mean that chest pain should be ignored.
In other words, the article itself would be considered deeply misleading, suggesting as it does that there is no reason to pay attention to chest pain.
Rebecca L. Dekker, PhD, RN, APRN has written an equivalently misleading article for Science and Sensibility, entitled What is the Evidence for Induction for Low Amniotic Fluid in a Healthy Pregnancy?
She claims to be answering the following question:
Low fluid seems to be the new “big baby” for pushing for induction. What does the research say about low fluid at or near term? From what I’ve been able to see in research summaries at least, there appears to be no improved outcome for babies, but I’d love to see the research really hashed out…
Decker writes:
There is no evidence that inducing labor for isolated oligohydramnios at term has any beneficial impact on mother or infant outcomes.
But that’s not what the questioner asked. She asked about oligohydramnios, not about isolated oligohydramnios. Decker does not even bother to answer the actual question since that would require acknowledging that there is plenty of scientific evidence that oligohydramnios can lead to perinatal death and poor outcomes. Instead, she decides to address a subset of cases of oligohydramnios while never making it clear that this is what she is doing.
There’s a big difference between oligohydramnios and isolated oligohydramnios. In this context, isolated means oligohydramnios in women who have NO other abnormalities, NO underlying risk factors, NO complicating conditions AND normal test results. No one ever claimed that every case of oligohydramnios is a sign of impending disaster, but that doesn’t mean that oligohydramnios should be ignored. To the contrary, it should be investigated vigorously.
As Zhang et al. point out in an paper on isolated oligohydramnios:
It is well established that oligohydramnios is associated with a high risk of adverse perinatal outcomes. On the other hand, oligohydramnios is a poor predictor for adverse outcomes.11,12 An explanation for these seemingly conflicting observations lies in the fact that not all oligohydramnios are the same. Our study shows that oligohydramnios with unfavourable maternal and/or fetal conditions (such as IUGR, anomalies or hypertension) leads to a much worse perinatal outcome than a normal amniotic fluid volume with the same conditions. In these cases, oligohydramnios may be an indicator of a more severe impaired placental function, fetal compromise and worse maternal/fetal conditions. However, we found in the current study that about half of the oligohydramnios cases did not have any coexisting medical or obstetric conditions. Fetuses in these cases tend to be appropriately sized at the diagnosis of isolated oligohydramnios. More importantly, with advancing gestation, their growth does not seem to be impaired… (my emphasis)
Dekker employs the classic NCB technique for deliberately misleading women: the bait and switch. She poses one question (what does research say about oligohydramnios), but answers another, different question (what does research say about isolated oligohydramnios, a subset of all cases of oligohydramnios).
Oligohydramnios is a symptom. As such, it requires investigation to determine whether there are other abnormalities such as fetal growth restriction, maternal hypertension, etc. If any additional symptoms or complicating conditions are found, induction is often the appropriate treatment to reduce the risk of perinatal death. Only IF the search for other symptoms and complicating conditions has revealed NOTHING ELSE can we conclude that there is no need for induction.
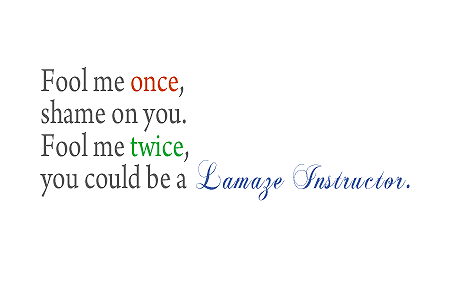
Dekker should be ashamed of herself for writing such a deliberately misleading article and Science and Sensibility should be embarrassed to publish it. But I suspect neither will be moved, since it appears that deliberately misleading women is a central element of natural childbirth advocacy. When there is no scientific evidence to support your position, the only way to convince women is the bait and switch.