The American Journal of Obstetrics and Gynecology has just published a “Report of Major Impact” that demonstrates that electronic fetal monitoring saves lives.
Electronic fetal heart rate monitoring and its relationship to neonatal and infant mortality in the United States by Chen et al. is the largest study ever done on electronic fetal monitoring (EFM). The authors reviewed 1,732,211 singleton live births (elective C-sections and congenital anomalies were excluded. Of these births); 89% involved EFM while 11% did not. They found:
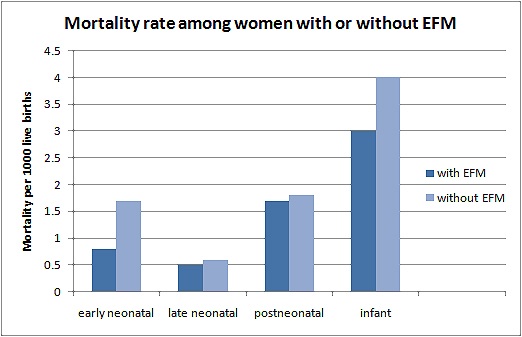
The corrected early neonatal, late neonatal, postneonatal, and infant mortality rates for all subjects were 0.9, 0.5, 1.7, and 3.1 per 1000 births, respectively… The risk of corrected mortality rate was different between those with vs without EFM during the early neonatal period (0.8 vs 1.7 per 1000 births, respectively; P ‹ .001), but not in late (0.5 vs 0.6; P ‹ .402) or postneonatal periods (1.7 vs 1.8; P ‹ .296).
In other words, EFM cut the rate of early neonatal death in half (death from birth to 7 days), but had no impact on late neonatal death (from 7-28 days of life) or postneonatal death (from 1 month to 1 year of age). This is exactly what you would expect to find if EFM prevents peripartum death from hypoxia (lack of oxygen). The results are represented graphically below.
There were secondary findings as well:
… Use of EFM was associated with an increased likelihood of operative vaginal delivery for all indications, as well as for fetal distress. In addition, use of continuous monitoring was associated with an increased risk of primary cesarean delivery for fetal distress …
…[U]se of EFM was associated with a lower likelihood of 5-minute Apgar score ‹4…
The secondary analysis also indicates that the rate of neonatal seizure was significantly lower only among high-risk women who had EFM…
What are the differences between this study and the Cochrane review that purported to show that EFM increases operative delivery rates without improving neonatal survival? The Cochrane review, encompassing 37,000 women, was simply too small.
The combined sample size of 12 RCTs is insufficient to determine whether EFM can significantly lower neonatal mortality. Alfirevic [the author of the Cochrane review] noted that to test the hypothesis that continuous monitoring can prevent 1 death in 1000 births, more than 50,000 women need randomization…
Moreover, as the Cochrane review authors themselves noted, of the 12 RCTs included in the analysis, only 2 were high quality studies.
Chen et al. conclude:
According to the Cochrane review and the most recent ACOG recommendation, the use of fetal heart rate monitoring increases operative delivery rate without a concomitant decrease in longterm neonatal outcomes. Thus, understandably there has been continued angst about using fetal heart rate monitoring during labor. The main implication of our study is that now there is reassuring evidence for the use of EFM; its use is linked with … a significant decrease in early neonatal and infant mortality … [F]etal heart rate monitoring can be used in daily practice with some assurance.
A conclusion of the study is the large sample size necessary to demonstrate improvement in neonatal outcomes. One reason the … Cochrane review did not demonstrate benefit of EFM is small sample size of published reports. Alfirevic et al acknowledged that over 50,000 women need to be randomized to demonstrate improvement in mortality. The issue of sufficient sample size … remains unachievable in modern day obstetrics… Thus, when the outcomes are uncommon and randomized trials are not plausible, we should consider evidence from “reality-based medicine,” for it, along with this study, demonstrates improvement in mortality
with EFM.
Of note, this study, which contains only live births, almost certainly underestimates the benefit of EFM. EFM appears to save lives by decreasing the risks of hypoxic brain injuries associated with low Apgar scores (‹4). The study did not include intrapartum deaths (Apgar 0), where the benefits of EFM are similar or even larger.
The bottom line is that the largest study of electronic fetal monitoring to date shows that EFM cuts the rate of early neonatal death in half. That is a dramatic benefit.